Background: Risk factors for Clostridium difficile infection (CDI) include antibiotic use, prolonged hospitalization, cancer chemotherapy, hematopoietic stem cell transplantation (HSCT) and gastric acid suppression, all of which, are encountered in acute leukemia patients. We sought to examine the impact of CDI on inpatient outcomes and resource utilization, as well as, to evaluate the trends of CDI in acute leukemia patients.
Methods: The Nationwide Inpatient Sample (NIS) database was queried to include all adults with acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML), who were admitted between 2012 and 2017 for inpatient chemotherapy and/or hematopoietic stem cell transplant (HSCT). Those with and without CDI were compared. T-test was used to compare means of continuous variables and chi-square test to compare proportions of categorical variables. Multivariable logistic regression was used to evaluate risk factors for CDI, as well as, inpatient mortality. Statistical tests for trends of resource utilization across six years were performed.
Results: A total of 187,105 admissions met the inclusion criteria, of which, 5.3% had CDI. Mean age (51.3 years) and gender (male 56.4%) did not significantly differ between those with and without CDI. AML accounted for a larger proportion of the CDI group (72.4% vs 64.6%, p<0.0001). CDI was associated with higher rates of inpatient mortality (8.9% vs 4.4%), ICU-level care (8.5% vs 3.7%), shock (9.6% vs 3.6%) and acute kidney injury (21.2% vs 11.1%), p<0.0001 for all outcomes.
On multivariate analysis, independent risk factors for CDI included: AML, HSCT, neutropenia, higher comorbidity burden (in the form of Charlson comorbidity index) and being treated at a teaching hospital. Blacks had lower rates of CDI. After adjusting for demographic variables, comorbidities, and accounting for higher proportion of AML, HSCT and neutropenia in the CDI group, CDI still accounted for higher risk for inpatient mortality (aOR 1.76, 95% CI 1.48-2.10, p<0.001), increased length of stay by 9 days (95% CI: 8.0-10.1, p<0.001) and higher hospitalization charges by around $33k per admission (95% CI: $25k-39k, p<0.001).
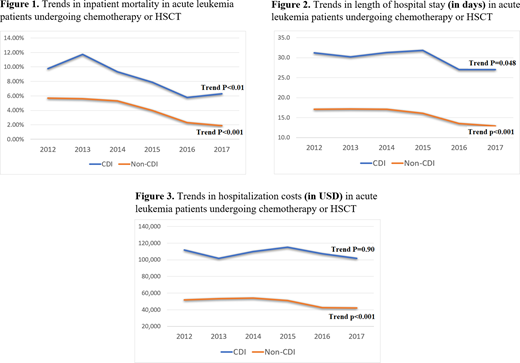
CDI rate in acute leukemia patients remained stable between 2012 to 2017. The mortality rates declined in both groups (9.8% in 2012 to 6.3% in 2017, p<0.01 in the CDI group and 5.7% in 2012 to 1.9% in 2017, p<0.001 in the non-CDI group). Similarly, length of hospital stay improved in both groups (31 to 27 days in CDI group, p=0.04 and 17 to 13 days in non-CDI group, p<0.001). While the hospitalization costs improved significantly in the non-CDI group ($52k to $42k, p<0.001), there was no statistically significant change in the CDI group ($112k to 102k, p=0.90).
Conclusions: CDI has a substantial impact on outcomes in acute leukemia patients. Higher incidence of CDI in HSCT recipients may be explained by prolonged hospitalizations, increased antibiotic exposures, and extended periods of impaired host immunity. Additionally, GVHD may also play a role in the incidence of CDI and its outcomes. Despite improvement in outcomes over the years, mortality rates and financial burden of CDI on health care, is still substantially higher in those without CDI, therefore, there is a need to focus on preventive measures.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal